Glaucoma Treatment in Lucknow
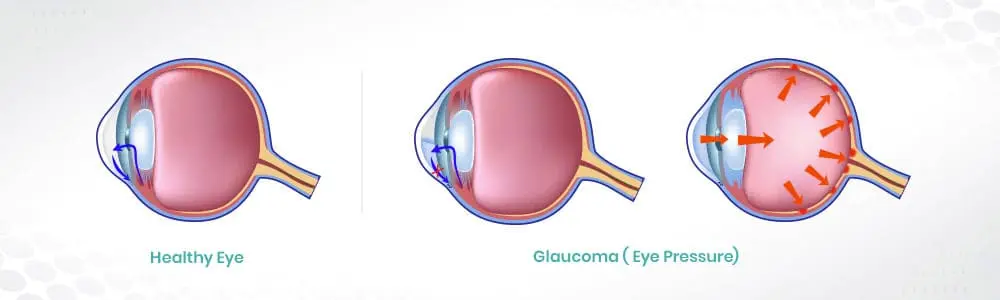
Glaucoma is a group of eye conditions that damage the optic nerve, usually due to increased pressure within the eye. It’s a leading cause of irreversible blindness worldwide. The optic nerve is responsible for transmitting visual information from the eye to the brain, and damage to this nerve can result in vision loss and, if untreated, blindness.
One of the primary risk factors for glaucoma is elevated intraocular pressure. However, not all cases of glaucoma are associated with high pressure, and some individuals can develop the condition even with normal eye pressure.
There are different types of glaucoma, including primary open-angle glaucoma (POAG), angle-closure glaucoma, normal-tension glaucoma, and secondary glaucoma. POAG is the most common type.
In the early stages, glaucoma often develops without noticeable symptoms or pain. Vision loss usually starts with peripheral vision and can progress gradually over time. In advanced stages, individuals might experience tunnel vision or even complete loss of vision.
Factors such as age, family history, high intraocular pressure, certain medical conditions (like diabetes or hypertension), and ethnic background can increase the risk of developing glaucoma.
Regular eye exams that include measurement of intraocular pressure, examination of the optic nerve, and visual field testing are essential for detecting glaucoma. Early detection and treatment can help prevent vision loss.
While there’s no cure for glaucoma, treatments aim to lower intraocular pressure to prevent further damage to the optic nerve. Treatment options include eye drops, oral medications, laser therapy, or surgery, depending on the severity and type of glaucoma.
After glaucoma surgery, it’s essential to follow your doctor’s instructions carefully to promote healing and reduce the risk of complications. While specific guidelines might vary based on the type of glaucoma surgery performed and individual circumstances, here are some general precautions and things to avoid:
Rubbing or Touching Your Eyes: Avoid rubbing or touching your eyes, as this can disrupt the healing process and increase the risk of infection or complications.
Strenuous Activities: Refrain from engaging in strenuous activities or heavy lifting as advised by your doctor. Activities that increase intraocular pressure, such as heavy lifting or strenuous exercise, might interfere with the healing of the surgical site.
Water and Eye Exposure: Protect your eyes from water, particularly from getting directly into your eyes. Avoid swimming or activities that might expose your eyes to water, dust, or other potential irritants until your doctor advises it’s safe to do so.
Driving and Vision-Related Tasks: Initially, your vision might be blurry or compromised after surgery. Avoid driving or performing tasks that require clear vision until your doctor confirms that it’s safe for you to resume these activities.
Medications and Eye Drops: Follow your doctor’s instructions regarding the use of prescribed eye drops or medications. Ensure you administer them as directed for proper healing and to prevent infection.
Skipping Follow-up Appointments: Attend all scheduled follow-up appointments with your eye surgeon. These visits are crucial for monitoring your healing progress, assessing the surgical site, and adjusting treatment if necessary.
Over-the-Counter Medications: Avoid using over-the-counter medications or eye drops without consulting your doctor first, as they might interfere with the healing process or interact with prescribed medications.
The recovery period after glaucoma surgery can vary depending on the type of surgery performed, the individual’s overall health, and how well they follow post-operative care instructions. Here’s a general overview of the recovery process:
Immediate Post-Operative Period: Right after the surgery, patients might experience some discomfort, mild pain, or irritation in the eyes. The eyes might be sensitive to light, and vision might be blurry.
First Few Days: In the initial days following glaucoma surgery, it’s common to experience mild to moderate discomfort, redness, and a feeling of grittiness or irritation in the eyes. Eye drops and medications prescribed by the surgeon should be used as directed to aid healing and prevent infection.
Avoidance of Strenuous Activities: Patients are typically advised to avoid strenuous activities, heavy lifting, and bending over during the first week or as directed by their doctor. These activities can increase intraocular pressure and interfere with the healing process.
Follow-up Visits: Regular follow-up visits with the eye surgeon are crucial during the recovery period. These visits allow the surgeon to monitor healing, assess the surgical site, and adjust medications or treatments if necessary.
Gradual Improvement: Over the first few weeks, vision might gradually improve, although it could take some time for vision to stabilize completely. Some patients might notice improvements sooner than others, but it’s essential to be patient during the recovery process.
Return to Normal Activities: Patients are usually advised to avoid driving and strenuous activities for a certain period, depending on the type of surgery and the individual’s healing progress. Once the surgeon confirms it’s safe to do so, patients can gradually resume normal activities.
Long-Term Follow-up: While initial recovery might take a few weeks, long-term follow-up appointments with the surgeon are important to monitor eye pressure, assess vision, and ensure there are no complications or recurrence of glaucoma.
Glaucoma often develops gradually and might not cause noticeable symptoms in its early stages. It’s often referred to as the “silent thief of sight” because vision loss can occur without apparent warning signs until the condition has progressed significantly. However, there are several indicators and risk factors associated with glaucoma:
Elevated Intraocular Pressure (IOP): Increased pressure within the eye is a primary risk factor for glaucoma. However, not everyone with high eye pressure develops glaucoma, and some individuals can develop the condition with normal eye pressure.
Optic Nerve Damage: Glaucoma causes damage to the optic nerve, which is crucial for transmitting visual information from the eye to the brain. A thorough eye examination can reveal signs of optic nerve damage, such as changes in the appearance of the optic nerve head or thinning of the nerve fibers.
Visual Field Loss: In the later stages of glaucoma, individuals might experience peripheral vision loss, commonly known as tunnel vision. This occurs when the damage to the optic nerve progresses, affecting the visual field.
Increased Cup-to-Disc Ratio: During an eye examination, an ophthalmologist might observe an increased cup-to-disc ratio, which refers to the size of the optic cup (the hollow center of the optic nerve head) in relation to the optic disc. An increased ratio might indicate potential optic nerve damage.
Family History: A family history of glaucoma increases the risk of developing the condition. If a close family member, such as a parent or sibling, has glaucoma, it’s essential to be vigilant about regular eye examinations.
Age and Ethnicity: Advanced age, particularly being over 60, is a significant risk factor for glaucoma. Additionally, individuals of African, Hispanic, or Asian descent are at higher risk of developing certain types of glaucoma.
Other Factors: Conditions such as diabetes, hypertension, eye injuries, and long-term use of corticosteroid medications can also increase the risk of glaucoma.
